The waiting room at a modest family clinic in Santa Rosa, California, had already thinned out when a father and his teenage daughter took two quiet seats in the corner. He wore a blue polo and a practiced smile.
She wore a red hoodie and a look that didn’t lift from the floor. To the staff, the scene seemed unremarkable at first—appointment jitters, maybe a tough conversation ahead. But by night’s end, a routine visit would escalate into an urgent, deeply troubling case with two patients to protect: a 14-year-old and the baby she was carrying.
Their physician, Dr. Evan Laam, knew the family by sight. The father, Marco Halcón, lived just three houses down. But familiarity didn’t make what followed any easier.
When nurse assistant Rosa Delgado called the girl back for vitals, she noticed the first red flag: the father insisted on answering every question for his daughter—even her name.
Rosa redirected gently, but the girl, Lucia, kept her gaze pinned to her hands, fidgeting through every minute of the intake.
Back in the exam room, the father delivered it bluntly: “My daughter is pregnant.” The chart already hinted as much. Still, hearing it out loud, seeing the child shrink into her hoodie, made the air feel heavier, tighter.
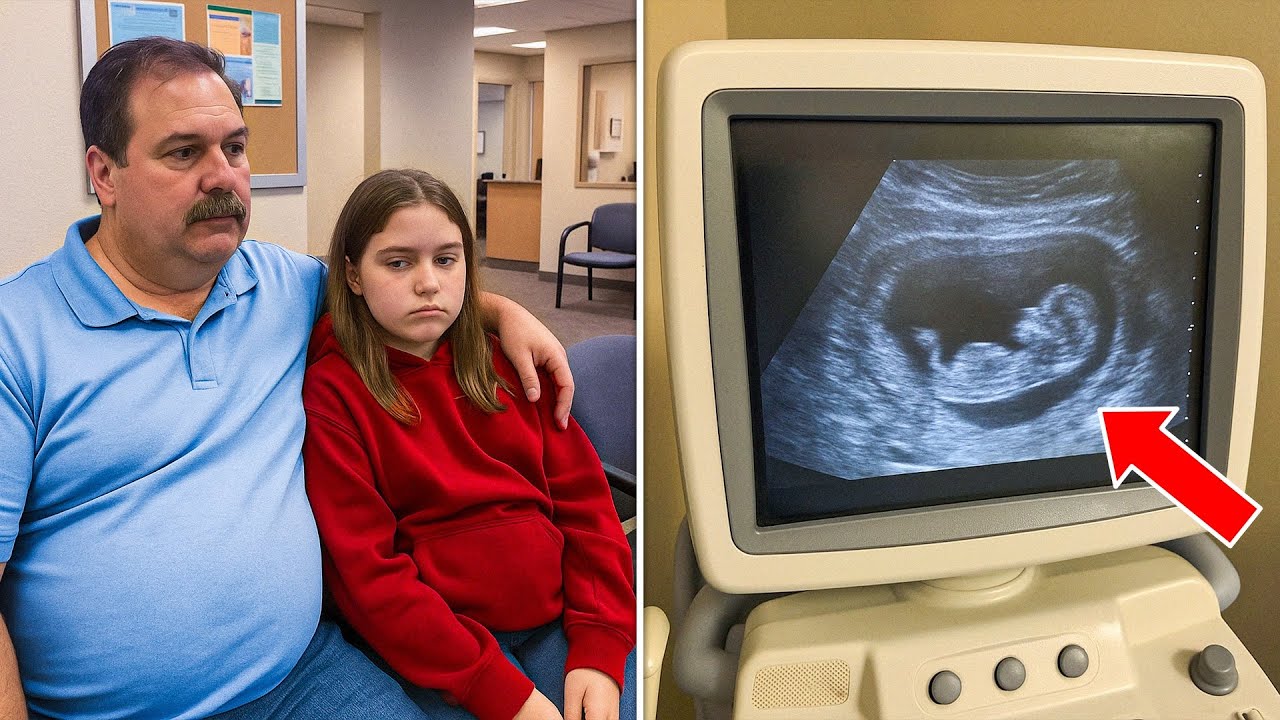
When Dr. Laam began the ultrasound, he expected what he always hopes for—reassurance. Instead, the grainy glow told a more complicated story.
“Twenty-eight weeks,” he said, adjusting the probe. That alone was startling—the pregnancy had been hidden for months without prenatal care. Then came the second shock. “I’m seeing signs of intrauterine growth restriction.” The baby’s measurements were behind where they should be, and the fetal heart rhythm skipped uncomfortably.
In plain terms: the unborn child was small, possibly struggling, and needed specialized monitoring—now.
The father pressed for a shortcut. “Can’t you just give her medicine?” No. This wasn’t a prescription problem; it was a hospital problem. Growth restriction and irregular heart patterns require tools small clinics don’t have—fetal Dopplers to evaluate blood flow, continuous monitoring, potential interventions, and the capacity to move fast if things turned.
The doctor wrote basic prescriptions for nutrition support—prenatal vitamins, folate, calcium—but delivered a firm instruction: go directly to the hospital.
Rosa began to clean the ultrasound gel from Lucia’s abdomen as the father stepped out to fill the prescription next door. That’s when the room shifted. The girl’s eyes welled. “She kicks when she hears his voice,” she whispered. “I hate that she likes him.”
The nurse and doctor exchanged a glance that said more than either could speak. Perhaps the words reflected a teenage storm of emotions. Perhaps they didn’t. Either way, they were a red flag—a chilling one. The moment passed as quickly as it came. The father returned. He guided the girl out with a firm hand on her shoulder. The clinic closed for the night. But the unease didn’t.
Driving home, the doctor spotted the family car in their driveway. Not the ER. Not the labor-and-delivery unit. He parked at his own house, tried to reason away the knot in his chest, and couldn’t.
Minutes later, he was on their porch, asking if they’d gone to the hospital. The father offered a new detail: the girl’s mother had taken her; he had work to finish. It was the first mention of a mother all evening.
Back at his desk, worry overcame etiquette. The physician searched for the mother online and sent a cautious message: I’m sorry to contact you this way, but I saw your daughter tonight. How is the hospital visit going? The reply came like a cold shock: What hospital visit? I haven’t seen my daughter in years.
In a single exchange, an already urgent medical situation became an emergency safeguarding case. The estranged mother, Daniela Rivera, had been out of her daughter’s life for a decade by court order, according to her account. The father’s claim that mother and daughter were at the hospital evaporated. The girl’s silence, the controlled answers, the plea wrapped inside that haunting line about the baby kicking—each detail slid into a grim alignment.
At this point, clinical caution must become action. In every state, healthcare providers are mandated reporters when they reasonably suspect abuse, exploitation, or neglect of a minor. That duty sits above discomfort, neighborhood ties, or fear of conflict. While patient confidentiality protects health information, it does not shield suspected harm to a child.
The immediate priorities are non-negotiable: ensure the minor’s safety, secure medical care for mother and fetus, and alert authorities trained to investigate.
That night in Santa Rosa, the path forward was clear: a welfare check, a rapid OB evaluation, and a multidisciplinary response. The medical urgency alone—28 weeks, suspected intrauterine growth restriction, and an irregular fetal heart—warranted urgent hospital care.
Growth-restricted fetuses face higher risks, from preterm birth to complications at delivery, and careful monitoring can make the difference between crisis and stabilization. For a 14-year-old, the stakes are higher still—body, brain, and emotions all under strain.
But the clinical picture was only half the story. The interpersonal dynamics inside that exam room raised alarms clinicians are trained to catch. A caregiver who insists on controlling all communication. A minor who avoids eye contact, defers automatically, and speaks only when the adult leaves.
A demand for secrecy—“No one can know”—that goes beyond ordinary privacy. A contradictory account about next steps. And then, that single, unforgettable sentence: a baby responding to a voice the mother fears. Each detail can be innocent. Together, they form a pattern.
What does a community do with a pattern like that? First, we listen—to nurses whose instincts often find what protocols miss, to doctors who refuse to rationalize the uneasy, to mothers cut out of the story who still answer the phone.
Second, we act—calling hotlines, asking hard questions, pushing past politeness when a child’s safety is on the line. And third, we learn the signs so we recognize them before the ultrasound screen turns urgent.
If you notice similar red flags—controlling behavior by a caregiver, a minor silenced in appointments, unexplained delays in urgent care—speak up. In the United States, the Childhelp National Child Abuse Hotline (1-800-4-A-CHILD) provides 24/7 confidential support. If someone is in immediate danger, call 911. For sexual assault support, the National Sexual Assault Hotline (800-656-HOPE) connects callers to local resources. These services exist precisely for nights like this one.
As for the girl in the red hoodie, her story is still being written. The facts we know emerge from a single evening in a neighborhood clinic: a physician who took a second look, a nurse who trusted her gut, an ultrasound that told the truth, a claim that didn’t hold up, and a mother who hadn’t been allowed to mother.
What comes next—medical stabilization, legal review, and a careful plan for safety—belongs to professionals tasked with protecting minors and the clinicians determined to stand beside them.
The lesson is simpler, and heavier. Sometimes the most important vital sign in an exam room isn’t on a monitor. It’s in a sentence spoken when the door closes and the loudest voice leaves. It’s the quiet truth a child manages to say, if only for a moment. The job—our job—is to hear it, to believe it matters, and to act before the screen goes dark.